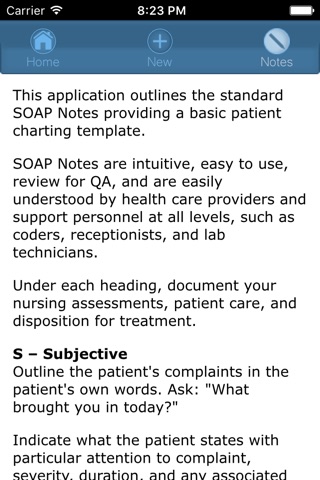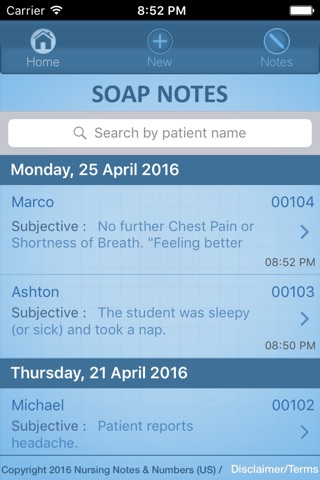
This application outlines the standard SOAP Notes providing a basic patient charting template.
SOAP Notes are intuitive, easy to use, review for QA, and are easily understood by health care providers and support personnel at all levels.
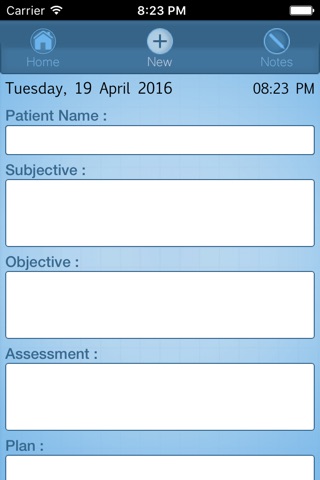
Under each heading, document your nursing assessments, patient care, and disposition for treatment. You can enter text or use the iOS voice function to add patient information.
S – Subjective
Outline the patients complaints in the patients own words. Ask: "What brought you in today?"
Indicate what the patient states with particular attention to complaint, severity, duration, and any associated problems.
For example, "Patient stomach pains described as cramping for 2 days. Complains of diarrhea for 1 day. Denies fever, nausea, or vomiting.”
O – Objective
Indicate your observations while listening to the patient and any examination you perform to assess the patients condition. Include age and gender. For example: “Patient female, 22. Patient guards right abdomen".
A – Assessment
Add your diagnostic nursing assessment. Include vital signs, any labs test results ordered, pain assessment on a scale of 1 to 10, and any physical assessment. For example, "RLQ tender upon palpation."
Do not offer diagnosis. Phrase assessment consistent with nursing diagnosis or assessment, for example, "Rule Out (R / O) Appendicitis."
P – Plan
Write your plan for treatment, referral, or other therapies.
Include any medications, additional diagnostics (radiographs) or subsequent labs tests you order. For example, “Order Liver Function Studies, Urinalysis (UA), or Occult Blood Test”.
If possible, indicate your plan for the patient throughout the continuum of care. For example, "Place patient in bed, refer to physician STAT, patient is NPO, follow-up and monitor vital signs every 15 minutes.”
Comments? Please contact us on FB at: https://www.facebook.com/Themobileclinician?ref=aymt_homepage_panel